Cyclospora cayetanensis: An Emergent Public Health Threat and an Enigma for Traceback Investigation
Unresolved or inconclusive epidemiology for several outbreaks offer compelling case studies of the challenges and risks posed by Cyclospora in food supply chains

In the world of parasitology, there are myriad "wee beasts" about which we have little or incomplete knowledge. Nonetheless, foodborne parasites are consequential risks for public health and food safety. Nearly 1.7 billion cases of diarrheal disease are reported globally every year, and the associated socioeconomic burden on health services has been estimated at 72.8 million disability-adjusted life years annually.1
Enteric protozoan parasites are among the major contributors to this diarrheal disease burden.2 According to the World Health Organization, roughly 25 percent of the global population is estimated to have an intestinal parasite infection, with the rate significantly higher in regions with poor sanitation and limited access to clean water. In these areas, infection rates can reach up to 50 percent of the population, meaning the "average human" has a moderate chance of harboring at least one intestinal parasite.2 Lower rates of infection are reported for industrialized nations, such as the U.S. Recent data indicate that these lower rates of infection are likely exacerbated when there are high rates of unsheltered people in the community. Lack of access to toilets and soap and hot water for hand hygiene are contributing factors in the increased spread of parasites. Since 1996 in the U.S., for example, the prevalence of Cyclospora cayetanensis has had an upward trajectory, trending toward endemicity. The parasites and other pathogens delivered to our food by the unwashed hands of humans are many.
Common and Neglected Foodborne/Waterborne Parasites: A Review
In the U.S., the most common foodborne and waterborne parasites include protozoa such as Cryptosporidium spp., Giardia intestinalis, C. cayetanensis, and Toxoplasma gondii; roundworms such as Trichinella spp. and Anisakis spp.; and tapeworms such as Diphyllobothrium spp. and Taenia spp.3 Many medically important parasites are also important agents of foodborne disease. T. gondii, for example, is a leading cause of foodborne disease deaths in the U.S. Studies from the mid- to late 2000s estimated toxoplasmosis to be the second-leading cause of deaths attributable to foodborne illness (an estimated 327 deaths) and the fourth-leading cause of hospitalizations attributable to foodborne illness (an estimated 4,428 hospitalizations). T. gondii infects an estimated 1.1 million persons each year in the U.S.4
The terminal host and other intermediate reservoirs for parasites are numerous and varied. Feline, porcine, ovine, and bovine animals, as well as fish and shellfish, are the frequently cited animal hosts.5,6,7 Medically important parasites are transferred to humans by a multitude of sources, routes, and modes. Contaminated water, fresh produce, berries, leafy greens, meat products, shellfish, and fish are frequently cited for this distinction.5 In fact, most food supply chains are vulnerable to attack and compromise by parasites.5,6,7 However, when food safety plans for most food companies are evaluated, it is noted that medically important, foodborne parasites have not been considered in the company's assessment of risk. Foodborne disease outbreak data, as presented here, seem to suggest that this is likely an important and potentially dangerous omission.
In general, most parasites have complicated lifecycles that include several stages of development and maturation.3,5,8–10 They reproduce by sexual and asexual means. The infectious form, for humans, is usually the oocyst; however, other developmental stages are reported to be capable of causing human disease.5,8 For example, the pork tapeworm Taenia solium causes two distinct diseases in humans.3,11 Both morbid processes, taeniasis and cysticercosis, are initiated by different stages in the cestode's development. Taeniasis is caused by the ingestion of the embryonated eggs passed in the stool of pigs or infected humans. Cysticercosis is a severe neurological condition that is caused by ingesting T. solium's larval stage.3,11
In the U.S., the Centers for Disease Control and Prevention (CDC) has classified cysticercosis as an important but neglected parasitic infection (NPI).13 This status is assigned to medically important parasites that produce severe illness, or that produce disease that presently cannot be prevented or treated. Cysticercosis, in humans, is most often initiated by the consumption of undercooked pork. Consuming improperly cooked bear meat has also resulted in this disease.3,11 The encysted larvae are contained within the host animal's muscle tissues—the structures that are frequently used as meat. In the small intestine, the larvae (cysticerci) emerge from their cysts, traverse the lumen of the small intestine, and thereby enter the circulatory system.11 Within the bloodstream, the larvae are circulated and delivered to the brain, eyes, and other organs. The diseases taeniasis and cysticercosis have very different pathologies.3,9,11 Taeniasis is relatively benign, whereas cysticercosis is debilitating and often fatal.11 In the early 19th century, it was thought that two separate and distinct organisms (parasites) were involved in these diseases. Cysticercosis, at the time, was reported to be caused by "bladder worms."11
C. cayetanensis and the Epidemiological Challenges of Parasitology
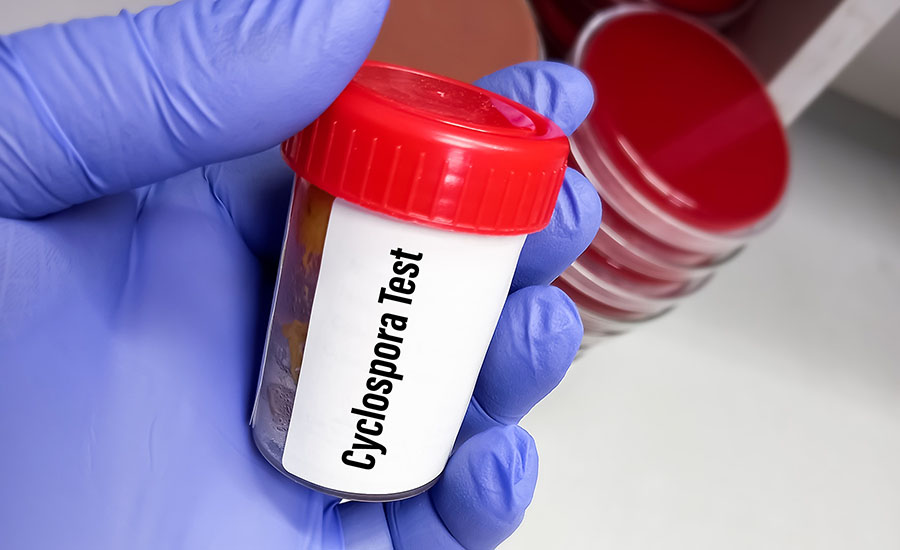
Parasitic organisms are exceedingly difficult to isolate and identify, which is a major challenge for those working with and attempting to diagnose parasitic diseases. Unlike bacteria and viruses, parasites are not culturable—i.e., they cannot be grown on artificial media for future harvest and study. Presumptive and differential diagnoses of parasitic diseases, in humans, are usually based on direct microscopic evidence obtained from stool specimens.5,6,9,10 Working with and preparing fecal matter for microscopic examination is both unpleasant and demanding of a high level of skill (Figure 1). Due to these challenges, it is reasonable to posit that failure rates in microscopic identification of parasites are relatively high. These failures would also contribute to inefficient or failed traceback efforts by the U.S. Food and Drug Administration (FDA), CDC, or other involved public health agencies.
Looking for quick answers on food safety topics?
Try Ask FSM, our new smart AI search tool.
Ask FSM →
The unresolved or inconclusive epidemiology for several major Cyclospora outbreaks occurring in 2023 offer compelling case studies of the challenges and risks posed by this parasite in food supply chains. For example, of the 24 major foodborne illness outbreaks investigated by FDA in 2023, four (17 percent) were attributed to Cyclospora cayetanensis.14,15 Of these four outbreaks, 75 percent were inconclusive in determining a food source.15 Broccoli was confirmed as the food source in the single outbreak investigation with conclusive epidemiological findings.2,14,15 The Cyclospora outbreak investigation data from 2022 and 2024 gave similar results.
In the annals of modern parasitology and foodborne disease, C. cayetanensis is a relative newcomer. This protozoan was first identified in 1979, in Papua New Guinea, as a parasite causing gastrointestinal disease in humans. It was initially mistaken for a coccidian parasite of the genus Isospora. The organism, later identified as Cyclospora cayetanensis, was initially unrecognized, and reports of diarrhea in travelers to Papua New Guinea, Haiti, and Mexico followed.4,8,16 Outbreaks of C. cayetanensis infections are frequently reported in developing countries with poorly developed sanitary infrastructure or in areas where the parasite is endemic.8,16 In recent years, C. cayetanensis has become an important global pathogen in humans.4,8,14 The parasite appears to be gaining endemicity in regions where it was virtually unknown less than 50 years ago.
The prevalence of reported Cyclospora infection in the U.S. has been low,14,16 possibly because many physicians are unfamiliar with its clinical features and the laboratory methods required for diagnostic confirmation. As noted previously, the primary method of diagnosis is by direct microscopy of human fecal material. Combined, these shortcomings in clinical and laboratory skills have likely resulted in an underestimation of the prevalence of Cyclospora-caused diarrheal disease in the U.S. CDC estimates that approximately 90 percent of cases in the U.S. are thought to be foodborne, amounting to an estimated 14,638 cases each year.14,16,17 This estimated annual case count data appears to be inconsistent with other reports from CDC, or perhaps these data are adjusted to reflect the high incidence of underreporting. Based on my review, laboratory-confirmed cases are typically an order of magnitude different than what is reported by CDC.
Past Cyclospora Outbreaks
A notorious outbreak of cyclosporiasis in 1986 was attributed to travelers returning to the U.S. from Mexico and Haiti. This episode marks the beginning of our understanding of Cyclospora as an agent of foodborne disease.4,14,16 The first outbreak reported to originate in North America occurred at a hospital in Chicago in 1990.4 That outbreak was linked to a contaminated rooftop water storage tank that supplied drinking water to the hospital's staff. CDC reports from this outbreak describe finding "small, spherical bodies" in the stool of those patients with diarrheal disease.14,16 With full benefit of retrospection, it is considered likely that the reliability of the assigned cause in the Chicago outbreak could be challenged. Cyclospora oocysts are shed into the environment in human excrement exclusively8—a fact that begs the important question: How did a rooftop water tank become contaminated with a human, fecal-borne parasite?
Another major outbreak in 1996 involving a total of 1,465 individual cases of cyclosporiasis was reported in the U.S. and Canada. Cases were distributed across 20 states, the District of Columbia, and the Canadian provinces of Ontario and Quebec.4,14 The only exposure that was consistently epidemiologically linked to Cyclospora infection was fresh raspberry consumption. Traceback studies of 29 events, for which adequate information was available, found the country of origin in every case was Guatemala.14 This event had a devastating impact on Guatemala's berry industry, nearly causing its collapse. In the years immediately following this outbreak, I moderated a session at a major food safety conference along with senior FDA Center for Food Safety and Applied Nutrition (CFSAN) officials to discuss traceback and traceability. During the session, the agency's officials came under heavy verbal attack by representatives of the Guatemalan berry industry. The Guatemalan protestors impugned the FDA's traceback findings as insufficient and inconclusive for assigning Guatemalan berries as the cause of the outbreak, and they questioned the validity and credibility of the agency's testing methods.
From 1997–2009, a total of 370 laboratory-confirmed cases of cyclosporiasis were reported in the U.S.14 The preponderance of these illnesses was reported in residents of Connecticut and Georgia. For this interval, positive stool specimens were collected nationwide, in all months of the year, with a peak in case counts occurring in June and July. This appearance of seasonality has also been reported by other researchers. Junqaing Li et al.18 report that, "Cyclospora infections are markedly seasonal, occurring in the rainy season or summer."
Vacation travel during summer may also contribute to this spike in cases. Approximately half of the U.S. cases reported during 2004–2009 were associated with international travel.14,16,17 As exemplified by the 1996 outbreak, traceback involving parasites can be enigmatic. Detection methods, to date, are based on oocyst morphology, staining, and molecular testing. Wet mount preparations and contrast staining techniques are the standard microscopic methods of identification. In wet mount preparations, the thick-walled, spherical oocyst measures 8–10 micrometers in diameter.5,16 Even today, armed with more sophisticated methods of analysis and greater knowledge about Cyclospora, CDC and FDA continue to be challenged when conducting traceback studies for outbreaks in which Cyclospora spp. are implicated.4 This is a great challenge for public health and a paradox for traceback investigations.
The Lifecycle of Cyclospora
Cyclospora is a genus of Apicomplexan parasites. The large phylum Apicomplexa are among the most prevalent and morbidity-causing pathogens worldwide.17,19 It includes the species C. cayetanensis, the causative agent of cyclosporiasis.19 Members of Cyclospora are characterized as having oocysts with two sporocysts, each containing two sporozoites. The overall prevalence of C. cayetanensis in humans worldwide is reported at 3.55 percent. C. cayetanensis is an important global pathogen in humans, typically causing prolonged diarrhea accompanied by anorexia, malaise, nausea and cramping, among other symptoms.8,17 It is estimated that the interval from infection to identification and confirmation of the disease is approximately 3–6 weeks.17,19,20 While the onset of symptoms has been reported to be abrupt in most adult patients, the incubation period ranges from 1–11 days.17,20 The at-risk population includes both immunocompetent and immunocompromised individuals.16,17,20 The disease is self-limiting in most immunocompetent patients, but it may manifest as severe, protracted, or chronic diarrhea in some cases, and may colonize extra-intestinal organs in immunocompromised patients.23,24
Cyclospora's primary mode of transmission involves a fecal–oral mechanism; soiled, contaminated hands in the mouth. However, with C. cayetanensis, direct hand-to-mouth infection does not normally occur because its unsporulated oocysts, as first passed in human stool, are not immediately infectious.19,20 The oocysts become infective in the environment only after undergoing sporulation. Under ideal conditions (23 °C to 27 °C), sporulation occurs within 7–14 days.4,20 It has also been reported that oocysts, in the environment, can survive freezing temperatures. Food and water contaminated with the sporulated oocysts are common vectors in their transmission.4
A great deal is known about this parasite; however, the lifecycle of C. cayetanensis has not been fully elucidated. The oocyst is the only stage definitively identified.4 Cyclospora has both sexual and asexual modes of reproduction occurring in the small bowel of humans.4,20,22 The ingested oocysts undergo excystation in the small intestine. The newly emerged sporozoites (1.2 μm × 9 μm) invade the intestinal lining. Sporozoites lack the crystalloid or refractile bodies that are primary differentiating characteristics of the oocyst.4,17 The sporozoites are immediate progenitors of unsporulated oocysts. When the oocyst is excreted in human stool, it is an undifferentiated sphere containing a morula. The oocyst has a bilayered wall. A polar body and oocyst residuum are also present. C. cayetanensis oocysts also exhibit auto-fluorescence.4,16,20,21 In wet mount preparations, the oocysts appear as bright blue circles under UV light with an excitation filter within the range of 330–380 nm.21 According to the Public Health Agency of Canada, the infectious dose (10–100 oocysts) for Cyclospora is considered very low.
The oocysts are very stable in the environment. They are capable of survival and sporulation under the normal extremes of environmental temperatures. In studies to confirm temperature sensitivity, it was shown that the oocysts were inactivated when they were exposed to extreme temperatures. No sporulation was observed at −70 °C, 70 °C, and 100 °C for oocysts contained in water samples, and there was no sporulation when dairy products were cooked at 70 °C, frozen at −70 °C for 1 hour, or after exposure to −15 °C for 24 hours.22,26 Thus, thorough cooking of suspect foods to internal temperatures greater than 70 °C or freezing at –15 °C for 24 hours could be used to mitigate the threat of illness caused by this pathogen. It is noted, however, that the viability of most food items that have been implicated in disease outbreaks caused by Cyclospora are not compatible with such harsh treatments.
Although chlorine and other antimicrobial chemical treatments are effective at reducing harmful populations of bacteria and viruses, they are not considered effective against C. cayetanensis.24,25 In countries or geographic regions where cyclosporiasis is endemic, microfiltration, ozone, or UV treatments may be necessary to effectively decrease populations of C. cayetanensis in irrigation waters.15,24–26 Plasma-activated water (PAW) is currently being investigated for this application. High-power ultrasound has also shown efficacy in this application.
Cyclospora Infection and Human Hygiene
In areas where there is a lack of access to toilets, soap, hot water, and other hygiene facilities, there is also a corresponding increase in reported rates of open defecation, leading to an increased risk of unsporulated Cyclospora oocysts in the natural environment. From 2022 to January 2024, the population of unsheltered persons in the U.S. increased by 31 percent.28 By 2024, the unhoused or unsheltered population in the U.S. was estimated at approximately 800,000 individuals.28 It is also acknowledged, by those reporting these data, that these numbers are likely inaccurate. The actual number could be more than 1 million individuals.
The massive increase in the unsheltered population occurs concurrently with the significant rise in the number of cases of cyclosporiasis reported in the U.S. According to a 2019 National Institute of Health (NIH) report, unhygienic practices (open defecation) were reported as causal factors in deadly hepatitis A virus outbreaks among unsheltered populations in both California and Michigan (2016–2018).30 A 2025 report from Multnomah Public Health found a sharp increase in cases of shigellosis over a seven-year period, with 19 cases in 2017 and 158 cases in 2024.31 The same report also revealed a spike in the numbers of unsheltered people (in the study area) occurring over the same interval. The researchers reported 4,177 cases of homelessness in 2017 and nearly 6,500 cases in 2024.31 The authors of the report linked the spike in disease to a lack of access to toilets, hot water, and soap for the unsheltered population. The diseases—cyclosporiasis, hepatitis A, and shigellosis—all share fecal–oral routes as their primary mode of infection. Logically, it follows that an increase in Cyclospora oocysts in the environment will result in more cases of cyclosporiasis. A Monte Carlo simulation is not required for predicting this outcome. Simply put, more opportunities for exposure will result in greater acquisition of the parasite and more disease.
Foods frequently implicated in Cyclospora outbreaks include berries, cilantro, and basil. These crops are harvested during late spring and early summer and correspond with the seasonality of outbreaks that are reported for Cyclospora.11,12 Moreover, cilantro is a hand-harvested crop, which magnifies the potential risk of on-farm contamination (Figure 2). Good agricultural practices (GAPs) can be used to avoid this hazard.

Good hand hygiene is also an important measure in preventing the spread of Cyclospora. While direct hand-to-mouth infection does not occur due to the need of the parasite to sporulate, it is possible that contaminated hands might deposit the unsporulated oocyst onto a food's surface, where the oocysts then undergo sporulation. The fresh produce section of the supermarket is an ideal setting for this mode of contamination. An individual with soiled hands could possibly contaminate a large quantity of fruits and vegetables during a single trip to the market. Moreover, as previously reported, fresh produce is frequently implicated in outbreaks caused by Cyclospora. Under this scenario, conducting a successful traceback study would be nearly impossible.
Endemicity of Cyclospora in the U.S.
The endemicity of Cyclospora in the U.S. has yet to be confirmed; however, it does appear to be trending in that direction. In 2019, FDA and CDC created the Cyclospora Task Force to address the increase in outbreaks, as well as the emergence of C. cayetanensis in domestically grown produce.31 In recent years, the number of domestically reported cases of cyclosporiasis has steadily increased. The number of cases more than doubled from 537 in 2016 to 1,194 in 2017, and then nearly tripled to 3,519 cases in 2018. In 2019, 4,703 cyclosporiasis cases were reported.25 In an August 2023 report from NIH,32 it was noted that for the period 2019–2022, the number of laboratory-confirmed cases of cyclosporiasis in the U.S. ranged from a high in 2019 of 2,408 cases to a low in 2021 of 1,024 cases. The NIH report also confirmed that the disease outbreaks, for that interval, were widespread and reported by more than 30 states. Once again, most of the outbreaks, according to the NIH report, occurred during the early spring and summer months. It was also noted that many of the reported outbreaks did not involve international travel, indicating that Cyclospora has become established in the U.S. population.
As of November 2023, the U.S. has experienced four major Cyclospora outbreaks involving 2,272 laboratory-confirmed cases with 186 individuals hospitalized due to complications of the disease.30 The cases were reported across 40 states, and none of the ill persons reported international travel in the 14 days prior to the onset of their illness. By the end of November 2023, CDC had proclaimed an end to the outbreaks.33 It is striking, however, that the agency has also reported that, "No specific cause of these illnesses was identified." The foods or beverages that may have been involved in causing these outbreaks are unknown. This lack of epidemiological certainty represents a great challenge for public health and for the food processing industry—especially for the fresh produce sector, as history has shown fresh fruits and vegetables to be at greatest risk of Cyclospora contamination. The supply chains for fresh produce are long, and there are many opportunities for contamination between harvest and point-of-sale. Those nodes at which human handling is required are the most vulnerable.
At the farm, for example, it is possible that contamination could result from direct contact with human fecal material. There are reports to confirm open defecation occurring on farms when the availability and accessibility of toilet facilities are inadequate. The risk of contamination by soiled hands, within sorting and grading sheds, is also considered high. Likewise, at the point of sale (i.e., in the supermarket display case), fresh produce is at extreme risk of contamination due to the consumer habit of hand manipulation—touching, feeling, or squeezing various items of produce prior to purchase. This point-of-sale mode of contamination is exacerbated in high-volume, high-traffic supermarkets. Most supermarkets do not have safeguards in place that would curtail direct hand contact with produce.
In a recent development, following the COVID-19 pandemic, some markets provide sanitizing wipes in their shopping cart storage areas (Figure 3). It appears that the wipes are intended for cleaning shopping baskets, not hands. The number of times an item of food is touched by human hands at the market is likely incalculable; so, too, then, is the risk of contamination by Cyclospora or other fecal-borne pathogens. Traceback activities conducted by CDC and FDA are often flummoxed by this supply chain complexity. For example, the two agencies have not been able to assign cause for the nearly 2,300 cases of cyclosporiasis occurring in the U.S. during 2023.

Over the years, I have often seen it reported that hand hygiene is the best and most cost-effective public health intervention for preventing the spread of disease in human populations. Yet, according to CDC, it is estimated that global rates of handwashing after using the toilet are only 19 percent. In the U.S., only 78.5 percent of the total population washes their hands regularly, and only 33 percent of the population uses soap and water when washing their hands.35 Worldwide, on an annual basis, about 1.8 million children under the age of five die from diarrheal diseases and pneumonia. Much of this disease burden is attributed to poor handwashing.
CDC reports that handwashing education can have profound effects for improving the health of a given community. Effective handwashing has been shown to achieve the following:33
- Reduces the number of people who get sick with diarrhea by 23–40 percent
- Reduces diarrheal illness in people with weakened immune systems by 58 percent
- Reduces respiratory illnesses, like colds, in the general population by 16–21 percent
- Can prevent up to 1 million deaths from preventable diseases each year.
The trend line for foodborne parasitic disease, in the U.S. and other countries, appears to be in the upward direction. This is especially true for cyclosporiasis. Since those initial outbreaks first reported in the 1990s, there have been year-over-year increases in the number of outbreaks. In 2017, there were 597 cases in 36 states; in 2018, there were 2,299 cases in 33 states; in 2019, there were 2,408 cases in 37 states; and in 2020, the case count was 1,441 with 34 states reporting the disease.
In response to the 2020 outbreak of cyclosporiasis associated with bagged salad mix, FDA investigated two Florida farms identified through traceback in its attempt to determine the source of the contamination. FDA investigators analyzed water samples from a regional water management canal located west of Port St. Lucie, Florida. The agency reported that all of its samples tested positive for C. cayetanensis. During a follow-up study, FDA collected additional creek and canal samples from nine unique locations. C. cayetanensis was identified in 89 percent of the samples tested. Even with this high rate of positive samples, FDA was unable to confirm that the C. cayetanensis detected in its water samples were a genetic match to the clinical isolates obtained from the outbreak and, as a result, could not conclusively determine the source of the outbreak.36 It is interesting to note the very high prevalence (90 percent) of Cyclospora in the surface waters that were evaluated by FDA. These data are very strong indicators that Cyclospora has reached the point of endemicity in this environment. This is an important finding insofar as what it might portend for the future of food crops grown in this region and in the U.S. more broadly.
Summary and Takeaway
Cyclosporiasis is a gastrointestinal disease characterized by debilitating, persistent, and recurring watery diarrhea. The symptoms typically appear 2–14 days after exposure. Some patients also present with abdominal cramps, severe vomiting, weight loss, low-grade fever, muscle aches, and prostration. There is also evidence that some in the population are asymptomatic when infected by this parasite. Both immunocompetent and immunocompromised individuals are at risk of this disease. In some cases, hospitalization is required. For example, during the 2023 outbreak involving 2,300 cases, approximately 8 percent of those infected required hospitalization. CDC and FDA both report that the incidence of cyclosporiasis in the U.S. is grossly underreported. The agencies suggest that most infected individuals do not report illness or seek medical treatment. Again, the source of the parasite is human excreta exclusively. Contaminated human hands play a critical role in the transmission of Cyclospora and numerous other foodborne pathogens. Shigellosis, a bacterial disease, offers an excellent example of another gastrointestinal disease initiated by this hand-to-mouth mechanism.
By 2023, there were nearly 3,000 cases of cyclosporiasis reported in the U.S. Likewise, the number of states reporting outbreaks has also continued to increase. As of late October 2023, 41 jurisdictions, including 40 states and New York City, reported a total of 2,272 laboratory-confirmed cases of cyclosporiasis. It is also important to note that the affected individuals in those cases had not traveled outside of the U.S. during the 14 days before they became ill. The reasons for the apparent trend towards endemicity for Cyclospora in the U.S. are not clear. More precise traceback data from the various outbreaks could enable our understanding of this emerging public health issue and of its endemicity. However, to date in the U.S., most Cyclospora outbreaks have gone without definitive epidemiological findings. The source of most outbreaks remains an unknown. For the outbreaks occurring in 2023 and 2024 involving more than 3,000 cases, none of the epidemiological studies from FDA and CDC have been definitive in their determination of the modes or methods of disease transmission. These processes remain an unresolved mystery.
It is known that Cyclospora's oocyst must incubate in the environment for a period of 7–14 days before sporulating and becoming infectious. Current knowledge indicates that humans are the only source of the oocysts in the environment. Humans are the parasite's definitive host. Many researchers have reported the apparent seasonality of cyclosporiasis. They report an uptick in the number of outbreaks occurring in late spring and summer. The increase in outbreaks also corresponds with the harvesting time for several food items that have been previously implicated in outbreaks. Leafy greens, berries, cilantro, broccoli, basil, and other herbs are all harvested during this pre-summer interval; hence, it is entirely plausible that many outbreaks have an on-farm connection. Unsanitary practices by farm workers, including open defecation in the fields or direct hand contact with the crop items during sorting, grading, and packing operations, are a few examples of possible contamination routes. Good agricultural practices on the farm are paramount in preventing the spread of the parasite into food supply chains.
Another prominent and high-risk node in the supply chain is the supermarket. Fresh fruits and vegetables displayed in this setting are vulnerable to contamination from the hands of prospective consumers. CDC and FDA data show that nearly 20 percent of the U.S. population do not properly wash their hands after using the toilet. Consumers, as a matter of habit, will touch and feel raw fruits and vegetables prior to making a purchase. This habit exposes the produce to whatever contaminants may be on the consumers' hands, including fecal matter. This insidious form of contamination is widespread across the country. Moreover, from a traceback standpoint, this is the worst-case scenario, as it is virtually impossible to track and trace a disease outbreak under these conditions. More aggressive intervention at the supermarket might be helpful in preventing or reducing the number of future outbreaks. Hand cleaning stations or hand dips installed in the produce section of the store, or the provision of disposable gloves at the produce display case, might influence shopper behavior and result in a positive outcome for public health. Education and outreach programs by public health agencies, focused on improved hand hygiene, are also important.
As stated, human beings are the sole source of C. cayetanensis oocysts in the environment; thus, all Cyclospora outbreaks are attributable to a human being. Regarding unsheltered persons, it is important to note that this population does not have regular and proper access to sanitary facilities, toilets, soap, and hot water. The unhoused population in the U.S. may comprise 1 million or more individuals. By necessity, unsheltered persons add human waste to the environment, and they do not have proper access to hygiene. This growing population may be another important factor in Cyclospora's gains toward endemicity in the U.S. over the past 50 years.
Cyclosporiasis is considered an "important neglected parasitic infection" by CDC. It is also a nationally notifiable disease. Cyclospora is an emergent foodborne pathogen that is frequently overlooked in risk assessments for food safety assurance—an oversight that might not be justifiable.
References
- U.S. Centers for Disease Control and Prevention (CDC). "What Causes Parasitic Diseases." July 12, 2024. https://www.cdc.gov/parasites/causes/index.html.
- Torgerson, P.R., B. Devleesschauwer, N. Praet, et al. "World Health Organization Estimates of the Global and Regional Disease Burden of 11 Foodborne Parasitic Diseases, 2010: A Data Synthesis." PLOS Medicine 12, no. 12 (December 2015). https://pubmed.ncbi.nlm.nih.gov/26633705/.
- CDC. "About Human Tapeworm." June 13, 2024. https://www.cdc.gov/taeniasis/about/index.html.
- Jones, J.L., M.E. Parise, and A.E. Fiore. "Neglected Parasitic Infections in the United States: Toxoplasmosis." American Journal of Tropical Medicine and Hygiene 90, no. 5 (May 2014): 794–799. https://pmc.ncbi.nlm.nih.gov/articles/PMC4015566/#:~:text=In%20the%20United%20States%2C%20studies,an%20estimated%204%2C428%20hospitalizations)%2C%20and.
- Keener, L. "Medically Important Foodborne Parasites: A Consequential Challenge for Food Safety Assurance." Food Safety Magazine April/May 2024. https://www.food-safety.com/articles/9390-medically-important-foodborne-parasites-a-consequential-challenge-for-food-safety-assurance.
- Keener, L. "Foodborne Parasites: An Insidious Threat to Food Safety and Public Health." TrainCan Inc. October 12, 2021. https://www.traincan.com/foodsafetynews/foodborne-parasites-an-insidious-threat-to-food-safety-and-public-health.
- Keener, L. and T. Koutchma. "Survey of Preventive Measures for Controlling Foodborne Parasites." Food Safety Magazine December 2021/January 2022. https://www.food-safety.com/articles/7476-survey-of-preventive-measures-for-controlling-foodborne-parasites.
- Li, J., R. Wang, Y. Chen, L. Xiao, and L. Zhang. "Cyclospora cayetanensis infection in humans: Biological characteristics, clinical features, epidemiology, detection method and treatment." Parasitology 147, no. 2 (February 2020): 160–170. https://pmc.ncbi.nlm.nih.gov/articles/PMC10317703/.
- Moss, M.O. and M.R. Adams. Food Microbiology. Royal Society of Chemistry, 1995.
- Motarjemi, Y., et al. Emerging Foodborne Pathogens. CRC Press, 2006.
- "Cysticercus." Wikipedia. https://en.wikipedia.org/wiki/Cysticercus.
- Nobel, E.R. and G.A. Nobel. Parasitology—The Biology of Animal Parasites. 4th Ed. Lea & Febiger, 1976.
- Parise, M.E., P.J. Hotez, and L. Slutsker. "Neglected Parasitic Infections in the United States: Needs and Opportunities." American Journal of Tropical Medicine and Hygiene 90, no. 5 (May 2014): 783–785. https://pmc.ncbi.nlm.nih.gov/articles/PMC4015562/.
- CDC. "Surveillance of Cyclosporiasis." July 16, 2025. https://www.cdc.gov/cyclosporiasis/php/surveillance/index.html#:~:text=Cyclosporiasis%20is%20a%20nationally%20notifiable,cyclosporiasis%20in%20the%20United%20States.
- Ortega, Y.R. and R. Sanchez. "Update on Cyclospora cayetanensis, a Food-Borne and Waterborne Parasite." Clinical Microbiology Reviews 23, no. 1 (January 2010): 218–234. https://pmc.ncbi.nlm.nih.gov/articles/PMC2806662/.
- CDC. "Notes from the Field: Doubling of Cyclosporiasis Cases Partially Attributable to a Salad Kit—Florida, 2021–2022." Morbidity and Mortality Weekly Report 72, no. 27 (July 7, 2023): 751–752. https://www.cdc.gov/mmwr/volumes/72/wr/mm7227a3.htm.
- Fleming, C.A., D. Caron, J.E. Gunn, et al. "A Foodborne Outbreak of Cyclospora cayetanensis at a Wedding: Clinical Features and Risk Factors for Illness." JAMA Internal Medicine 158, no. 10 (1998). https://jamanetwork.com/journals/jamainternalmedicine/fullarticle/205859.
- Li, J., R. Wang, Y. Chen, L. Xiao, and L. Zhang. "Cyclospora cayetanensis infection in humans: Biological characteristics, clinical features, epidemiology, detection method and treatment." Parasitology 147, no. 2 (February 2020): 160–170. https://pmc.ncbi.nlm.nih.gov/articles/PMC10317703/.
- Dixon, B., B. Mihaljlovic, H. Couture, and J.M. Farber. "Qualitative Risk Assessment: Cyclospora cayetanensis on Fresh Raspberries and Blackberries Imported into Canada." Food Protection Trends 36, no. 1 (January 2016): 18–32. https://www.foodprotection.org/publications/food-protection-trends/archive/2016-01-qualitative-risk-assessment-cyclospora-cayetanensis-on-fresh-raspberries-and-blackberries-im/.
- CDC. "Cyclosporiasis." https://www.cdc.gov/dpdx/cyclosporiasis/index.html.
- Seeber, F. and S. Steinfelder. "Recent advances in understanding apicomplexan parasites." F1000 Research 5 (June 2016). https://pmc.ncbi.nlm.nih.gov/articles/PMC4909106/.
- "Cyclospora." Wikipedia. https://en.wikipedia.org/wiki/Cyclospora#:~:text=Cyclospora%20is%20a%20genus%20of,sporocysts%2C%20each%20containing%20two%20sporozoites.
- Li, J., R. Wang, Y. Chen, L. Xiao, and L. Zhang. "Cyclospora cayetanensis infection in humans: Biological characteristics, clinical features, epidemiology, detection method and treatment." Parasitology 147, no. 2 (February 2020): 160–170. https://pmc.ncbi.nlm.nih.gov/articles/PMC10317703/.
- Li, J., R. Wang, Y. Chen, L. Xiao, and L. Zhang. "Cyclospora cayetanensis infection in humans: Biological characteristics, clinical features, epidemiology, detection method and treatment." Parasitology 147, no. 2 (February 2020): 160–170. https://pmc.ncbi.nlm.nih.gov/articles/PMC10317703/.
- Berlin, O.G.W., J.B. Peter, C. Gagne, C.N. Conteas, and L.R. Ash. "Autofluorescence and the Detection of Cyclospora oocysts." Emerging Infectious Diseases 4, no. 1 (March 1998). https://wwwnc.cdc.gov/eid/article/4/1/98-0121_article.
- Rogers, E.L., J. Arida, J. Grocholl, J. Njoroge, and S. Almeria. "Detectability and Persistence of Cyclospora cayetanensis Oocysts in Artificially Contaminated Soil and Fresh Herbs Grown Under Controlled Climatic Conditions." Pathogens 14, no. 5 (April 2025). https://www.mdpi.com/2076-0817/14/5/430.
- U.S. Food and Drug Administration (FDA). "Constituent Update: FDA Shares Updates on Cyclospora Prevention and Research Efforts." Current as of July 25, 2022. https://www.fda.gov/food/hfp-constituent-updates/fda-shares-updates-cyclospora-prevention-and-research-efforts.
- Soucy, D., M. Janes, and A. Hall. "State of Homelessness: 2024 Edition." National Alliance to End Homelessness. August 5, 2024. https://endhomelessness.org/state-of-homelessness/.
- Clark, S. "Dysentery Outbreak Hits Oregon." March 6, 2025. Newsweek. https://www.newsweek.com/dysentery-outbreak-hits-oregon-2040727.
- Peak, C.M., S.S. Stous, J.M. Healy, et al. "Homelessness and Hepatitis A—San Diego County, 2016–2018." Clinical Infectious Diseases 71, no. 1 (June 2020): 14–21. https://pubmed.ncbi.nlm.nih.gov/31412358/.
- FDA. "Investigations of Foodborne Illness Outbreaks." https://www.fda.gov/food/outbreaks-foodborne-illness/investigations-foodborne-illness-outbreaks.
- Almeria, S. L. Chacin-Bonilla, J.G. Maloney, and M. Santin. "Cyclospora cayetanensis: A Perspective (2020–2023) with Emphasis on Epidemiology and Detection Methods." Microorganisms 11, no. 9 (August 2023): 2171. https://pubmed.ncbi.nlm.nih.gov/37764015/.
- CDC. "Surveillance of Cyclosporiasis." July 16, 2025. https://www.cdc.gov/cyclosporiasis/php/surveillance/index.html.
- FDA. "Cyclospora Prevention, Response and Research Action Plan." Current as of June 30, 2023. https://www.fda.gov/food/foodborne-pathogens/cyclospora-prevention-response-and-research-action-plan.
- Peysakhovich, R. "51 Hand Washing Statistics & Facts." Cleango. https://www.bookcleango.com/blog/51-hand-washing-statistics-facts.
- Viazis, S., F. Shakir, A. Straily, A. Goodrich-Doctor, J.L. Sumter, and S. Trujillo. "Outbreak Investigations of Cyclospora cayetanensis Infections 2013–2020: Progress Made and Challenges Remaining." Food Safety Magazine April/May 2022. https://www.food-safety.com/articles/7675-outbreak-investigations-of-cyclospora-cayetanensis-infections-20132020-progress-made-and-challenges-remaining.
Larry Keener, CFS, PA is President and CEO of International Product Safety Consultants. He is also a member of the Editorial Advisory Board of Food Safety Magazine.