Global Efforts to Prevent Antibiotic-Resistant Foodborne Pathogens in Developing Countries
The World Organization for Animal Health (OIE) recently reported that 45 countries (among 155 countries that participated in its survey between 2015 and 2017) still use antibiotics for growth promotion in animals (Figure 1). Modern agriculture is associated with an increase in the use of antimicrobials (antibiotics). The responsible use of antibiotics is important to ensure food safety and food security. However, the inappropriate, unnecessary, and overuse (70% of the global increase in antibiotic use in food animals, in the next two decades, will be in developing countries) of antibiotics in food-producing animals has significantly jeopardized their effects by creating antibiotic-resistant bacteria.
 The current world population is about 7.6 billion people and is projected to reach about 10.0 billion people by 2050. To feed all of these people, global agricultural production must increase by 60 percent by 2050. Furthermore, increasing incomes in developing countries have been associated with an increased demand for high-value food products including food animals (meat, eggs, milk, and dairy products), fruits, and vegetables. In developing countries, most of the agricultural production increases will come from increasing yields and/or increasing crops. Modern agricultural intensification (i.e., the overcrowding of animals/plants, especially in conjunction with poor farming practices) is associated with increase antibiotic use.
The current world population is about 7.6 billion people and is projected to reach about 10.0 billion people by 2050. To feed all of these people, global agricultural production must increase by 60 percent by 2050. Furthermore, increasing incomes in developing countries have been associated with an increased demand for high-value food products including food animals (meat, eggs, milk, and dairy products), fruits, and vegetables. In developing countries, most of the agricultural production increases will come from increasing yields and/or increasing crops. Modern agricultural intensification (i.e., the overcrowding of animals/plants, especially in conjunction with poor farming practices) is associated with increase antibiotic use.
In developing countries, antibiotics are available over the counter through unregulated supply chains. Total antibiotic use in food-producing animals will exceed 200,000 tons in 2030. It is expected that about 70 percent [99% in countries such as Brazil, India, and China (the largest antibiotic consumer)] of the global increase in antibiotic use in food animals over the next two decades will be in developing countries.
Today, in some countries, the use of antibiotics in food-producing animals (cattle, poultry, swine, etc.) is 3–4 times higher than used by people. Antibiotics are used in food-producing animals to a) treat infected animals (disease treatment), b) prevent illness in healthy animals when infected animals are present (metaphylactic uses or disease control), c) prevent illness in animals when no infected animals are present (prophylactic uses), and d) growth promotion (production-purpose uses). Growth-promoting antibiotics are normally given to increase feed efficiency/weight gain where animals can be exposed to low doses over a long period of time, which can lead to the development of resistant bacteria.
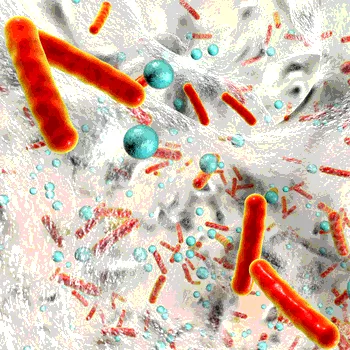
Antibiotic resistance is the ability of bacteria to resist the effects of antibiotics. Food animals are considered one of the most important reservoirs of antibiotic-resistant foodborne pathogens (e.g., Campylobacter, Salmonella, Escherichia coli, etc.), which can be transmitted to humans via the consumption of contaminated food or direct contact with infected animals via their feces, urine, saliva, or blood. Farmers, food handlers and their families, and consumers are among the most people at risk of being infected with antibiotic-resistant bacteria. In developing countries, direct and indirect transmission of antibiotic-resistant foodborne pathogens are equally important because food safety systems are weak or do not exist, and humans interact frequently with animals and their environment [manure (many developing countries use raw/improperly treated human and animal waste as fertilizer), soils, water, etc.]. High levels of antibiotics-resistant foodborne pathogens have been isolated from many developing countries including Brazil, China, Egypt, Indonesia, Thailand, Tunisia, South Africa, etc.
Antibiotic-resistant infections kill about 700,000 people a year worldwide and is expected to reach 10 million people per year by 2050. For example, in the European Union, more than 25,000 people die from infections caused by antibiotic-resistant bacteria each year. In the U.S., according to the U.S. Centers for Disease Control and Prevention, antibiotic-resistant Salmonella (spreads from animals to people mostly through food) causes about 100,000 infections every year. Antibiotic-resistant Campylobacter (spread from animals to people through contaminated food, especially raw or undercooked chicken) causes more than 300,000 infections every year. Antibiotic-resistant Shigella (spreads in feces through direct contact or through contaminated surfaces, food, or water) causes about 27,000 infections each year. Antibiotic-resistant bacteria cause more than 23,000 deaths each year in the U.S.
The reduction of antibiotic resistance is crucial in protecting human, animal, plant, and environmental health. Therefore, international health organizations have developed monitoring programs to address antibiotic resistance in the food chain. The Food and Agriculture Organization, the OIE and the World Health Organization (WHO) have collaborated to address antimicrobial resistance in the food chain. The WHO recently developed guidelines for developed and developing countries to control the spread of antibiotic-resistant organisms. The OIE recently reported positive global progress on the regulation and monitoring of antimicrobial use in animals, reporting that many countries have already taken key actions on the use of antimicrobials in human and animal health. For example, the number of countries that do not have a regulatory framework on the use of growth promoters was reduced from 110 (prior to 2015) to 72 (by 2017). The use of antimicrobials for growth promotion has declined globally from 60 (prior to 2015) to 45 countries (by 2017). However, critically important antibiotics continue to be used in food-producing animals in several regions.
Developed countries, including the U.S., Canada, Denmark, France, Japan, Norway, and Sweden, have developed and implemented programs to monitor the use of antibiotic in animal and food products. In the U.S., the U.S. Food and Drug Administration (FDA) started, in 1977, efforts to ban the use of antibiotics in growth promotion, achieving the Veterinary Feed Directive rule of 2017. According to FDA, in the U.S, sales and distribution of all medically important antibiotics intended for use in food-producing animals decreased by 33 percent between 2016 and 2017. In Norway, a decrease of about 40 percent of antibiotic use in animals was achieved in the last two decades. In the European Union, antibiotics use for growth promotion were banned in 2006. Developing countries, including Mexico, Ethiopia, Brazil, China, India, and Thailand, have also started to develop/implement policies and guidelines to control the spread of antibiotic-resistant bacteria (see “Recommendations for Developing Countries”). Therefore, developed and developing countries must work together to avoid human, environmental, and economic costs of antibiotics resistance.
Barakat Mahmoud, Ph.D., was an associate professor of food safety at Mississippi State University. He has provided technical assistance in food safety in several developing countries in Africa, Asia, Central America, and the Caribbean.
Looking for quick answers on food safety topics?
Try Ask FSM, our new smart AI search tool.
Ask FSM →








